BIOMECHANICS OF ABSORBABLE IMPLANTS
Abstract
The present paper addresses topics on the use of biodegradable implants in trauma orthopedic surgeries, from its development to clinical application. It is also underlines the non-necessity of a new surgical procedure for its removal, since these implants are disintegrated and eliminated by the organism after the fracture consolidation, especially in the case of children.
Keywords
Absorbable Implants; Polyglycolic Acid; Internal Fixation of Fractures; Intramedullary Fixation of Fractures
Over the last decades, the metallic devices for ostheosynthesis, such as screws, plates and nails have made possible a technical improvement, as well as being efficient and safe in the surgical treatment of orthopedic trauma injuries.1
However, metallic implants are still associated to some adverse effects, such as wire migration, growth abnormalities, difficulty in radiology visualization due to implant white-out, infection, cellularity effects and rigid fixation that could cause bone atrophy. Sometimes, in areas with anatomic singularities where the subcutaneous tissue is scarce or due to the proximity to tendons, implants would need to be removed, being that case a must in children when considering their exponential bone growth.
Mittal et al2, in a questionnaire distributed to 100 adult patients with fractures, asked subjects how they would like to have their fractures fixed: 95% responded it could be done with bioabsorbable material and 80% would be willing to take part of clinical studies comparing metallic with bioabsorbable materials.
The latter has been a reason for researchers to investigate bioabsorbable implants, not for them to be substituted, but to become an extra option in the instrumental apparatus for the surgical treatment of injuries in orthopedic traumatology.
Bioabsorbable implants should be sufficiently resistant to guarantee the maintenance of the fracture reduction and fixation (osteotomy) during the consolidation period, thus progressively degrading itself.
These materials should also be body-friendly, with no carcinogenic, teratogenic, toxic, inflammatory or allergic effects.
Review of the Literature
-Phases of development
The absorbable synthetic structures have been clinically used for more than 20 years.2
The first study with biodegradable implants was carried out in 1996 by Kulkarni et al3, analyzing the biocompatibility of the poly-L-lactic acid (PLLA) in animals, which showed to be non-toxic and that could gradually degrade itself. In 1971, the same author made evident the use of plates and screws made of PLLA in the fixation of canine jaws.
Since then, several studies have been conducted with biodegradable materials, being the 1990s a period when a great deal of publications emerged and when most of the investigations used the polyglycolic acid (PGA) and the polylactic acid (PLA) as instruments. Some innovations were introduced to enhance material resistance and improve biodegradation.
However, despite arduous research effort, the development of an ideal bioabsorbable implant for the fixation of fractures or osteotomy is still a heated debate.
The basic elements for the production of bioabsorbable implants are the polyglycolic and polylactic acids, which after polymerarization of the cyclic diesters, its outcome are polyglycolides and polylactides.
– Chemical properties
The polyglycolic acid (APG) and the polylactic acid (APL) are synthesized by the polymerization of the cyclical diesters from the glycolic and lactic acids.3
The polyglycolide (APG) is a crystalline polymer with a molecular weight ranging from 20,000 to 145,000.4 APG is hydrophilic and highly crystalized. Degradation and resistance loss occur prematurely, leading to post-surgical complications. In order to reach the point of deformability, its temperature must be over 36ºC/96.8ºF, and after decreased for application. This procedure is considered an issue, since surgical running time may take longer than planned. The suture threads made of polyglycolic acid have been commercially utilized since 1970.
The polylactide’s (APL) molecular weight ranges from 180,000 to 530,0005 and has an extra methyl group in its monomer (lactic acid), which makes it more hydrophobic.
The copolymers commonly used from the glycolic, lactic, such as polyglactin 910, are substances prepared by the polymerization of 9 glycolic parts and 1 lactic part. The copolymer obtained displays good fibrous properties and has also been used as a suture material since 1975.3
The copolymer self-reinforcement technique has led to better mechanical properties and eliminated toxic adhesion issues. The high degree of molecular orientation makes the implant rigid and strong in its longitudinal axis, allowing it to be compared with metallic implants. The microstructure of such materials is composed of a perpendicular bidirectional orientation, making the implant more resistant and deformable at the operating room’s temperature, avoiding the surgical procedures of warming and cooling. They also withstand a higher bending load and a lower memory effect (material tendency to return to its original form after bending), being their sterilization possible through gamma irradiation, which is not allowed in non-reinforced materials, since it would alter their mechanical properties.4-6
-Biodegradation
The degradation of polyglycolide and polylactide takes place in vitro and in vivo through hydrolisis, leading to a reduction of its mechanical properties. Degradation is faster in vivo.6
Craig et al7 have verified that the sutures made of polyglactin 910 were absorbed within 90 days.
Vainionpää8 has shown that pre-molded-beam-shaped pins made of polyglycolide are degraded in the cancellous bone within 12 weeks.
The outcome of the polyglycolide and polylactide degradation is used in the amino acid synthesis or in the tricarboxylic acid cycle.
The degradation final product is eliminated through urine, feces and exhaled as carbon dioxide, having the process complete, in rats, within 180 days.2
The factors that affect the implant biodegradation can be related to the implant itself – chemical composition, molecular weight, fiber orientation, monomer concentration, stereoisomerism, material phase, conformation, volume/surface rate, porosity, presence of impurities, sterilization methods and degradation mechanisms – or can be related to environmental factors – implantation place, type of tissue, implant stress and vascularization.
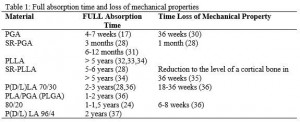
Table 1 shows the full time span of absorption and the loss of mechanical properties.
Source: Vainionpää S: Biodegradation of polyglicolic acid in bone tissue : an experimental study on rabbits. Arch Orthop Trauma; Surg. 104: 3338,1986.
– Tissue response
Hermann et al9 have compared the polyglycolide with other materials and observed a discreet inflammatory response in the use of polyglycolide and a sharper one with the use of a catgut or nylon.
Vainionpää8, in an experimental study with rabbits, has not observed a reaction or a foreign-body reaction to the polyglycolide.
Craig et al7 have reported a subtle hystological alteration, foreign-body reaction type, after the implantation of polylactide and polyglycolides sutures in the gluteal region of rats.
The discreet foreign-body reactions caused by bioabsorbable polymers have been considered, by several authors, as an initial biological response in the degradation evolution of bioabsorbable implants.10-12
– Internal fixation of the bone tissue with bioabsorbable implants
Mechanical properties
Törmälä et al13 have introduced the polyglactide pre-molded implants, which preliminarily were produced through mer copolymer modeling in metal, with a bending force of 45MPa and a tension force of 150MPa.
Based on these studies, the cylinder-shape bioabsorbable material nail was manufactured.
In the beginning, nails were made of polyglactine 910 with a resistance of 265 MPa.13 However, afterwards, due to better resistance value, nails made of polyglycolic acid were produced.
This type of nail was produced by using a reinforcement technique. Absorbable polymeric fibers were added in high temperature of the same polyglycoide material. By using this reinforcement with an initial resistance of 200-400 MPa, an inclination module of 220-400 MPa and a breaking resistance of 179-250 MPa have been obtained.13
In 1971, Frazza and Schmitt4 have shown that the initial tension force was reduced to half within a week, when sutures were implanted in the subcutaneous tissue of rats.
Nails made of polydioxanone present a low initial resistance, with a value of 92 MPa, which is reduced to around 50% within the first five weeks.14
– Experimental studies
The first experimental study on the use of bioabsorbable implants in the fixation of fractures was conducted by Cutright et al in 1971.15
In 1986, Vainionpää et al fixed osteotomy in the distal femur of rabbits with polyglycolic acid implants, associated to the trans bone suture of polyglycolide. Osteotomy was consolidated in all 19 rabbits. They have also observed bone formation within the canal, previously occupied by a pin, after the implant biodegradation. However, the device resistance was fairly weak for osteotomy fixation in the cortical bone.
In 198916, Mäkelä et al studied the fixation properties on physeal fractures of young rabbits and the effect of the bioabsorbable implant on the growth plate. It was concluded that a polydioxanone-2.0mm-diameter nail did not cause any growth disorder, although the 3.2mm-diameter nail caused a permanent damage to the rabbit’s distal growth plate.
In 198917, Vasenius et al investigated the resistance and properties of polyglycolic nails. It was shown that the nail resistance loss had lowered between 5 and 6 weeks in the rabbit’s subcutaneous tissue. Besides that, the resistance loss of polyglycolic nails is lowered faster in vivo than in vitro.
Elias et al11,19 have carried out a comparative experimental study with rabbits in which polyglycolic nails were assessed, comparing it to Kirschner wires, both with a 2mm diameter, transfixing the distal growth plate of the femur. It was concluded the bioabsorbable implants only caused a temporary growth disorder, since the growth plate caused the implant to break off between the sixth and seventh week after its implantation, which did not occur in the case of metallic pins.
-Clinical use of bioabsorbable implants
The first bioabsorbable implant for bone fixation, after experimental studies, was developed by Törmala et al (1987). The experimental studies have also foregrounded that the fixation properties of these implants suffice the fixation of osteotomies in the cancellous bone.8
The clinical application of bioabsorbable implants in malleolar fractures was first employed in 1984 by Rokkanen et al12, and then executed in various skeleton segments by other scholars.10, 11,15,19
In 1985, Rokkanen et al12 presented the result of a prospective randomized study on the fixation of ankle fractures utilizing bioabsorbable nails or metallic pins in 44 patients. No difference was found between the two groups.
In 1993, as a dissertation defended at the University of Helsinki, Partio et al14, in a clinical study with 318 patients (oleocranon and ankle fractures, and ankle fusion) presented good results for the use of nails and screws made of polyglycolic acid. It was reported that the foreign-body reaction type did not compromise the bone consolidation, besides showcasing some advantages on the use of bioabsorbable material: satisfactory consolidation, less pain, no need for material removal, reduction of hospital costs since it would not be necessary a subsequent hospitalization and anesthesia procedure. Other authors also corroborate with the latter.10-12,14,19
Elias et al11,18,19 have reported consolidation in all cases of elbow fractures in children and adolescents, fixed with bioabsorbable pins, and in ankle fractures of adults, fixed with bioabsorbable screws, with no loss of reduction or bone growth impairment. The occurrence of seroma was reported to be an issue in 8% of the cases, which besides sterile, has not interfered in the consolidation, which evolved to a cure after puncture.
Final considerations
The use of bioabsorbable implants is an extra option in the surgical treatment of fractures, fusions and osteotomies. It offers a psychological and economic advantage since a subsequent surgical procedure for implant removal is not needed, especially in the case of children.
More study on this matter is necessary to assess its long-run safety with regards to tentative collateral effects, such as carcinogenic and teratogenic ones.
The resistance of a bioabsorbable implant is still low, its application working best in diaphyseal bones, since in this region the consolidation takes place before it loses resistance, eventually degrading itself.
There are several research centers around the globe investigating bioabsorbable implants, being the Swiss Association for the Study of Osteosynthesis (AO) and the Tampere University of Technology, based in Finland, the ones that have invested on this matter.
References
1- Muller ME, Allgöver M, Schneider R, Willenegger H. Manual of internal fixation. Techniques recommended by the AO group. Second edition, 1-409, Springer-Verlag, Berlin, Heidelberg. New York,1979
2- Mittal R, Morley J , Dinopoulos H, Drakoulakis EG, Vermani E, Giannoudis PV. Use of Bioabsorbable implants for Stabilisation of distal radius fractures:The United Kingdom patients perspective. Injury. 2005; 36:333-8.
3- Kulkarni RK,Pani KC,Neuman C, Leonard F. Polyactic acid for surgical implants, Arch Surg. 1966; 93: 839-43.
4- Frazza EJ, Schimitt EE. A new absorbable suture .J Biomed Matter Res Symposium. 1971; 1: 43-58.
5- Ray JA, Doddi N, Regula D, Williams JA, Melveger A. Polydioxanone (PDS), a novel monofilament synthetic absorbable suture. Surg Gynecol Obstet. 1981; 153: 497-507.
6- Gilding D, Reed, AM. Biodegradable polymers for use in surgery-polyglicolic/polilatic acid homo and copolymers 1.Polymer. 1979; 20:1459-64.
7- Craig, PH; Willian,JA: A biologic comparison of polyglactin 910 and polyglicolic acid synthetic absorbable sutures. Surg Gynecol Obstet. 1975; 141:1-10.
8- Vainionpää S. Biodegradation of polyglicolic acid in bone tissue: an experimental study on rabbits. Arch Orthop Trauma Surg. 1986; 104: 333-8.
9- Herrmann JB, Kelly RJ,Higgins GA: Polyglicolic acid sutures. Laboratory and clinical evaluation of a new absorbable suture material. Arc Surg. 1970; 100:486-90.
10-Kontakis GM, Pagkalos JE, Tousonidis TI, Melissas J, Katonis P. Bioabsorbable materials in orthopaedics, Acta orthop Belg. 2007; 73: 159-169.
11-Elias, N. Adeodato, S. Jorge,FVF. O Uso de implantes bio-absorvíveis na Cirurgia Ortopédica. JBM. 1997; 73( 3): 35-7.
12-Rokkanen P, Böstman O, Vainionpää S, Vihtonen K, Törmälä P, Laiho J, et al. Biodegradable implants in fracture fixation: early results of treatment of fractures of the ankle. Lancet. 1985; I: 1422-4.
13-Törmälä P, Vainionpää S, Kilpikari J, Rokkanen P. The effects of fibre reinforcement and gold plating on the flexural and tensile strength of PGA/PLA copolymer materials in vitro. Biomaterials. 1987; 8: 42-5.
14-Partio EK, Böstman O, Vainionpää S, Pätiälä H, Hirvensalo E, Vihtonen K, et al. The treatment of cancellous bone fractures with biodegradable screws. Acta Orthop Scand Suppl. 1988; 59(227): 18.
15-Cutright DE, Hunsuck EE: The repair of fractures of the orbital floor using biodegradable polylatic acid. Oral Surg. 1972; 33: 28-34.
16-Mäkella EA, Mero M, Vainionpää S, Vihtonen K, Törmälä P, Rokkanen P. Trans physeal biodegradable fixation of experimental distal femoral physeal fractures in growing rabbits and cats. Book of abstracts,96, 8TH European Conference on Biomaterials. Heidelberg, Germany, September 7-9: 1989
17-Vasenius J, Vainionpää S, Vihtonen K, Mäkelä A, Rokkanen P, Mero M, et al. A comparison of in vitro hydrolysis, subcutaneous and intramedullary implantation to evaluate the strength retention of absorbable osteosynthesis implants. Biomaterials. 1990;11:501-4.
18-Elias N, Oliveira LP, Mesquita KC, Cordeiro DX. Transphyseal fixation. Comparative experimental study between biodegradable implants and metallic pins. Mapfre Méd 4 (Suppl II)1993: 281-2.
19-Elias, N; Oliveira LP, Mesquita KC. Fixação interna com implantes bio-absorvíveis das fraturas do cotovelo em crianças e adolescentes. Rev. Bras Ortop.1994; 29: 29-32.21
Attachments
Authors
Nelson Elias¹
1 Associate Professor – Rio de Janeiro State University – UERJ, 1989 – Assistant Orthopedics Professor.
Article received on March 30 2015
Article accepted on August 26 2015



