MUSCLE STRENGTH INCREASE IN OSTEOGENESIS IMPERFECTA WITH THE PILATES METHOD: A CASE STUDY
Abstract
Osteogenesis imperfecta is rare disorder of the connective tissue characterized by bone fragility and osteopenia, resulting in functional limitations and reduction in patient’s quality of life. The physical therapy works in the treatment and prevention by methods such as Pilates. The goal of this study was to understand the benefits of the Pilates method in the treatment of patients with OI. The evolution of the patient was analyzed during eleven months, based on medical records. The Pilates exercises were performed three times a week, with one-hour long sessions. Muscle strength, better body awareness and self-esteem gains are some of the benefits observed in present study.
Keywords: Osteogenesis Imperfecta; Muscle Strength; Postural Balance; Physical Therapy Modalities
Introduction
Osteogenesis imperfecta (OI), also known as brittle bone disease is a rare genetic disorder of the connective tissue, characterized by bone fragility and osteopenia with several clinical signs due to a deficiency of Type 1 collagen.1 Its variable clinical records may be synonym of functional limitation and reduction in the quality of life.2
OI treatment consists in keeping patients’ quality of life rather than reverse their health condition.3 Physical Therapy also works effectively on the treatment, mainly to prevent these patients fractures4 through kinesiotherapy, hydrotherapy and electrical stimulation as well as the Pilates method, the treatment proposed in this study.5
As in OI, patients suffering from osteoporosis develop bone brittleness and high chance of fractures. Therefore, such pathology must be considered, once its medication and physiotherapeutic treatments are similar to the OI one.
Osteoporosis is defined as an osteometabolic disorder reducing the bone mineral density, wearing out its structure and increasing fragility, rising the risks of fractures, which is the main clinical sign of the pathology. The practice of physical exercises is recommended for these patients’ treatment so as to minimize bone tissue losses and avoid possible falls, consequently improving balance, walking pattern, defense reactions and individual proprioception. In this context, Pilates is suggested as a therapeutic approach, with available records of its effectiveness in the improvement in the quality of life of the patients suffering from osteoporosis.6
The method is recommended for gain of flexibility, body definition and health improvement.7 Besides that, it also works posture awareness, corrects muscular imbalance and strengthens the muscles. Currently it is also known as a rehabilitation resource for the treatment of elite athletes, neurological disorders, chronic pain, orthopedic problems and low back pain.8
There are no studies relating Pilates to OI treatment in the literature so far. However, the practice of physical exercises is a well-known ally in the osteoporosis treatment, since muscular contraction increases bone density, strengthening this structure and decreasing the prevalence of fractures. Therefore, Pilates can be a therapeutic tool for OI treatment. It stimulates the production of calcium, strengthens tendons and joints, corrects posture alterations such as scoliosis, caused by bone deformities, develops the lung capacity and guides the patients on their daily acitivies.9
Case Report
Female patient, 34 years of age suffering from osteogenesis imperfecta type 4, showing a bluish sclerotic and a record of fractures as symptoms, aside from the short stature, 1.40m. Pilates practitioner from January to November 2014. Active, college student and part-time intern, she lives alone and is independent regarding her daily life activities.
She was born at 8 months of pregnancy, delivered in a normal childbirth with two bilateral femur fractures and bowing of the tibia and fibula. She would not crawl and started independent walking at 13 months of age. From that period on, a sequence of femur fractures started, fracturing the right femur, with an approximate frequency of one fracture per year.
Between 6 and 10 years of age, the number of fractures increased, raising to twice per year, allowing the installation of osteoporosis for lack of usage. In this time the patient used a HKAFO orthosis (with hips, knees and foot support) in order to help with her orthostasis.
After 10 years of age, she suffered 5 fractures, two in the same place of the tibia, one in the right fibula, and two in the femur, all due to the same trauma.
She underwent surgical procedures to fix a left femur fracture when she was 13 years old, having placed an intramedullary nail, being immobilized with plaster casting for 90 days.
According to her medical records, she suffered from ligamentous laxity, which made room for 3 sprains in the right ankle, all of them after she was 20 years old.
She evolved with a left knee dislocation, several lower limbs deformities due to the fractures and bones bowing. She presented osteopenia and osteoporosis in the right hip and in the spinal cord.
She was following drug treatment (Protos 2g) and medical follow up with an orthopedist and a psychologist.
The first contact of the patient with the Pilates method was in 2011 by medical recommendation. She practiced it for about one year, after stopping and resuming activities on January 6 of 2014, in the studio where the research was conducted. After a Physiotherapeutic Assessment, it was noticed that the patient suffered from a light pain condition in the right hip and in the lower limbs, more intense in the mean line of the left knee due to previous dislocation. At the physical examination, she presented anterior deviation of the head, depressed left shoulder blade, convex scoliosis to the right, an elevated right hip, genu varum, pronated feet, thoracic rectification and lumbar hyperlordosis, balance decrease reported to have become significantly worse, after the knee dislocation and a thoracic hypomobility.
In an assessment, described in her medical records, the Medical Research Council (MRC) Scale for Testing Muscle Strength was applied, obtaining as a result, a grade 3 for abdominal muscular and limbs strength.
Pilates classes were attended along the entire period from January to November 2014, 3 times a week, 60-minute long sessions, comprising this research conduction time.
According to the patient’s medical records, exercises were not performed on the Ladder Barrel, once the patient reported insecurity and fear of falling. The basic level exercises were preferably done on the ground level, always with a support base. They consisted of abdomen strengthening training, trunk side stretching at the Reformer and the Step Chair (Mermaid), strengthening of the lower and upper limbs done not only at the Cadillac, but also at the Reformer and the Step Chair, by also executing series such as Foot Work and Arm Springs with low resistance.
In the bimonthly records found, it is observed that the evolution of the exercises in this patient’s treatment followed the same parameters of any other training, gradually advancing as springs resistance was increased, with the association of other accessories to the exercises, along with an also gradual withdrawal of a supporting base.
In the bimonthly patient evolution recorded, the physiotherapist claims to have observed an improvement in the patient body awareness, a decrease in the left knee pain condition, and a slight gain of strength in the abdominal muscles.
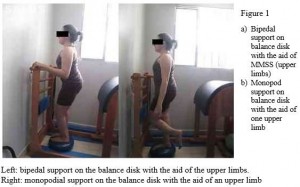
In the 3rd month of treatment the main goal was to improve balance and prevent falls. First stage exercises were maintained, and accessories were introduced for exercise load increase, like balance disks, roller or Swiss ball as a feet support in the Bridge exercise; or with the Magic Circle between the knees. Besides that, exercises like Single Leg Kicks wearing 1kg leg-pads in lower limbs, Foot Work on the Reformer, Leg Circles Educational exercises on the ground and The Cat to Elephant by the end of the class. The balance training on the disk was intensified during this phase, with monopod support on the disk with the aid of upper limbs.
By the end of the second bimester it was reported that the patient had achieved a better abdominal contraction, better posture awareness, and would do exercises on the ball with more control, besides managing to reduce shaking on the balance disk.
By the 5th month of treatment, it was reported that the patient was able to perform intermediate level exercises by increasing spring resistance, changing lower limbs position when doing exercises in dorsal decubitus, such as at The Hundred, with lower limbs at 90o and by removing the supporting base in the balance exercises.
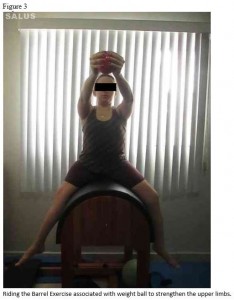
At the third bimester, the exercises were: Leg Circles, Proprioception works at the Reformer, doing Foot Work with the feet supported on the Swiss ball while the therapist would hold the ball, scapulothoracic dissociation at the Step Chair and Ball Diving, aside from those already executed to perfection by the patient in the initial phases. Barrel exercises were introduced, like quadriceps stretching, Riding, lower limbs posterior stretching and spinal cord extension in ventral decubitus. Reports revealed important gains in physical conditioning and resistance, muscular strength and balance, and also revealed that the patient reported an improvement in her daily life activities, performed with more vitality and in absence of pain.
At the 5th month treatment reassessment, the MRC Scale for Muscle Strength Scale was applied again: the strength grade went up to 4 in abdominal muscles and in lower and upper limbs.
Up to the seventh month, the previous level of exercises executed was maintained, with a load increase by using 2kg leg pads and springs with a higher tension. It was reported that the patient presented a better thoracic spine mobility, performing exercises without so much dependence on external feedback.
By the ninth month, the exercises were of an advanced level, aiming at the improvement of movements fluidity and quality. Some exercises performed were the Leg Pull Up and Down, Jack Knife, The Hundred on the Reformer, the Board with the upper limbs supported on the ball, and Rolling Down and Up with the Swiss ball. Patient evolution was reported in this phase of training, with a reduction in her muscle fatigue, observed when she would take on the advanced Teaser on the Cadillac.
Reports show that along the eleventh month, the sessions would flow better, allowing 20 exercises to be executed in a row without stopping. Sessions goals were to improve movement quality and fluidity, and add multitask capability with advanced level ground exercises, using a variety of accessories during the moves. Exercises such as The Teaser were performed, with resistance given accessories, glute kickbacks with Theraband resistance, Rows at the Cadillac on a dorsal decubitus position on the ball, quadriceps strengthening with associated upper limbs flexing movement with a Swiss ball in hand without any still point, and Jack Knife without the aid of the upper limbs. After the eleven-month training period the patient claimed: “Pilates has changed my life. I can’t live without it anymore”.
At the 11th month of treatment, the MRC Scale for Muscle Strength Scale was applied again: the strength grade went up to 5 in abdominal muscles and to 4 in lower and upper limbs.
In an unstructured interview about the changes occurred in the patient’s life, registered in her medical records, the patient claimed: “(…) I’ve gained in a lot of strength and balance and my joints are more stable. My posture is much better and I do not feel pain anymore”.
Discussion
Osteogenesis imperfecta (OI) is a rare genetic disorder of the connective tissue, characterized by bone fragility and osteopenia. It may be the synonym of functional limitation depending on its degree and clinical record in question.10
Concerning the Muscle Strength Grade, there was an increase in the upper and lower limbs strength between month 1 (one) and month 5 (five), evolving from Grade 3, in which the muscle only beats gravity, to Grade 4, in which the muscle copes with gravity and is able to face small resistance, degree kept until the last reassessment in month 11 (eleven). Therefore, there has been a 20% total strength gain to the upper limbs (MMSS) and to the lower limbs (MMII). It has been observed a 40% increase in the abdominal muscle strength, between January and November 2014, with an alteration from Grade 3 in the first month, to Grade 4 in the fifth month, and to Grade 5 in the eleventh month, which represents a normal abdominal muscle strength to face great resistance, as shown in Table 1.
The Pilates exercises are focused fundamentally on the core strength, aiming to align the trunk biomechanically, generating relief from the pain condition and health improvement, which contributes to this study since there was a reduction in the pain level in the lumbar spine region as reported by the patient.11
Abdominal muscles comprehend the main muscle group for the Pilates method. In all of its exercises, abdominal contraction is always associated with the movements, hence the great importance abdominal muscles play, together with the paravertebral muscles and the pelvic floor, in giving support to the postural alignment maintenance and to the action of defying gravity,12 confirmed here in this study, once it has been observed a fast abdominal strength gain by the patient studied.
This patient’s upper and lower limbs muscle strength increased and that may be related to the constant strengthening of upper limbs (MMSS) and lower limbs (MMII), gradually increasing spring resistance, as well as the usage of several accessories to enhance its activation, such as the Magic Circle and the Swiss Ball.13
The results found in this study corroborate with the findings from a 2012 research reporting on the importance of the centralization approach in the Pilates Method. There, the abdominal muscles are worked to stabilize the spinal cord, iliopsoas muscles, quadriceps, the lumbosacral region and the pelvic floor, in order to improve the muscle strength in the lower limbs, stabilize balance, and even improve the aerobic capacity, as a likely function of the increase in muscle tonus, thus reducing fatigue and improving muscle resistance to execute these tasks.14
Besides the quantitative gain previously mentioned, it was possible to observe a secondary qualitative gain, considering the patient’s improvement in self-esteem and quality of life, with anxiety reduction and adequate physical fitness, described by the patient as seen in her everyday life. Pilates is said by her to be “indispensable” to her physical and mental well-being. This effect may be related to the level rise of serotonin, epinephrine and dopamine, natural anti-depressants promoting the feeling of pleasure.15
Such benefits were also described by Joseph Pilates (1956), that affirmed: “Pilates develops the body uniformly (…) invigorates the mind and elevates the spirit”.
The pictures related to Pilates can be seen at the end of this paper.
References
- Santili C, Akkari M, Waisberg G, Bastos Júnior JO, Ferreira WM. Avaliação clínica, radiográfica e laboratorial de pacientes com Osteogênese imperfeita. Rev Assoc Med Bras. 2005;51(4):214-20.
- Kanno CM, Oliveira JA. Características clínicas e radiográficas da osteogênese imperfeita associada à dentinogênese imperfeita. Rev Odont. 2009;17(33):96-101.
- Maldonado VB, Silva FWGP, Filho PN, Consolaro A, Queiroz AM. Características clínicas da osteogênese imperfeita do tipo I e da dentinogênese imperfeita. Rev Paul Ped.2010;32(3):223-230.
- Assis MC, Plotkin H, Glorieux FH, Santili C. “Osteogenesis Imperfecta”: novos conceitos. Rev Bras Ortop. 2002;37(8):323-7.
- Moreira CLM, Lima MAFD, Cardoso MHCA, Junior SCSG, Lopes PB, Junior JCL. Determinantes da marcha independente na osteogênese imperfeita. Acta Ortop Bras. 2011; 19(5): 312-5.
- Brasil. Consenso brasileiro de osteoporose. Rev Bras Reumatol, [online], 2002; 42(6). Disponível em: http://www.osteoprotecao.com.br/pdf/consenso_brasileiro_osteoporose.pdf
- Silva ACLG, Mannrich G. Pilates na Reabilitação: uma revisão sistemática. Fisio Mov. 2009; 22(3): 449-455.
- Nogueira TRB, Oliveira GL, Oliveira TAP, Pagani MM, Silva JRV. Efeitos do método pilates nas adaptações neuromusculares e na composição corporal de adultos jovens. Revista Brasileira de Prescrição e Fisiologia do Exercício. 2014;8(45): 296-303.
- Brasil. Protocolo Clínico e Diretrizes Terapêuticas. Portaria de Osteogênese Imperfeita, nº 1.306, de 22 de novembro de 2013, Associação Brasileira de Osteogênese Imperfeita. [online]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/sas/2013/prt1306_22_11_2013.html
- Santili C, Akkari M, Waisberg G, Júnior JO, Ferreira WM. Avaliação clínica, radiográfica e laboratorial de pacientes com Osteogênese imperfeita. Rev Assoc Med Bras. 2005; 51(4): 214-20.
- Souza APGF, Ozana M, Vidigal J, Tinôco ALA, Martinho KO. Influência do Pilates e da Hidroginástica na qualidade de vida dos pacientes portadores de Osteoporose. Rev Cien Fed Int Educ Fís – FIEP [online]. 2011; 81. Disponível em: www.fiepbulietin.net.
- Sacco ICN, Andrade MS, Souza PS, Nisiyama M, Cantuária AL, Maeda FYI, et al. Método Pilates em revista: aspectos biomecânicos de movimentos específicos para reestruturação postural – Estudo de caso. R. bras. Ci. Mov.2005; 13(4):65-78.
- Comunello Jf. Benefícios do Método Pilates e sua Aplicação na Reabilitação. Instituto Salus. [online]. 2011. Disponível em: http://www.pilatesfisios.it/ricerche%20pdf/BENEFICIOS%20DO%20METODO%20PILATES.pdf
- Marés G, Oliveira KB, Piazza MC, Preis C, Neto LB. A importância da estabilização central no método Pilates: uma revisão sistemática. Fisioter. Mov. 2012; 25(2):445-51.
- Vieira JLL, Porcu M, Rocha PGM. A prática de exercícios físicos regulares como terapia complementar ao tratamento de mulheres com depressão. Jorn Bras Psiq [online]. 2015. Disponível em: http://www.scielo.br/pdf/jbpsiq/v56n1/a07v56n1.pdf>
Attachments
Table 1 – Scale for Testing Muscle Strength of the Medical Research Council
| Variation | % Variation MMII & MMSS | % Variation Abdominal |
| Month 1 to Month 5 | 20.00% | 20.00% |
| Month 5 to Month 11 | 0.00% | 20.00% |
| Month 1 to Month 11 | 20.00% | 40.00% |
Source: Patient Medical Records. Note: translated.
Authors
Amanda Cassilhas Trindade Mourrahy1; Mariângela Braga Pereira Nielsen2*
1Physical Therapist from School of Sciences of Santa Casa de Misericórdia – EMESCAM.
2 PhD in Kinesiology and PM&R (Physical Medicine and Rehabilitation) by Universidade Nacional de General San Martin – USAM, Argentina. Professor at School of Sciences of Santa Casa de Misericórdia – EMESCAM