EXCESSIVE DAYTIME SLEEPINESS IN SUBJECTS WITH SLEEP BREATHING DISORDERS
Abstract
Objectives: This study aimed at determining the prevalence of Excessive Daytime Sleepiness (EDS) in patients with sleep breathing disorders, as well as at investigating the sensitivity and specificity of the Epworth Scale to detect the Obstructive Sleep Apnea/Hypopnea Syndrome (OSAH); correlate the apnea-hypopnea index (AHI) and with the degree of EDS; age with the severity of OSAHS; the degree of excessive daytime sleepiness. Method: a cross-sectional study was carried out with a retrospective data collection, through medical analysis. The subjects were divided into two groups and three subgroups according to the AHI. The descriptive analysis was performed using mean, standard deviation, 2×2 tables, and statistics using the Pearson’s correlation. p Results: out of the 65 individuals studied, 68% were males with a mean age of 55.18 years, 34.31 AHI events/hour, and a score of 9.63 for the EDS. The EDS was prevalent in 52% of patients, particularly in the control group, depicting a low sensitivity in detecting the disease. By correlating the AHI with age, it was found a weak, negative and statistically significant correlation. Conclusion: the EDS proved to be prevalent in more than half of the population, though the Epworth Scale showed little sensitivity to OSAH and cannot, therefore, be solely used as a criterion for detecting the disease. It is worth highlighting the necessity of further studies on the matter to shed light on excessive daytime sleepiness, considering the latter is associated with the occurrence of accidents, morbidity, and has become a public health issue.
Introduction
Sleeping is considered a vital necessity for the human life. By playing a role of utmost importance for the preservation of the homeostatic conditions and for the physical and psychic functioning, its quality and amount are essential for the performance of brain and organic functions. Therefore, factors that interfere in sleeping pose a significant consequence on the subject’s life.1
According to Dal-Fabbro et al2, the Apnea Syndrome/Obstructive Sleep Apnea (OSAH) is one of the most prevalent sleep disorders in the population, being initially described in 1973 by Christian Guilleminault.
The OSAH is a clinical condition characterized by repetitive obstructions of the upper respiratory tracts (URT) due to a total (apnea) or partial (hypopnea) inspiratory collapse, leading to a decrease of oxygen serum levels and to an increase in the levels of carbon dioxide, resulting in micro wake ups, causing an impact on sleep quality and thus interfering in daily life activities.3,4
Abreu et al5 have also affirmed that the OSAH is associated with the development of systemic arterial hypertension and an array of other cardiovascular conditions, such as congestive heart failure, arrhythmia, heart disease and cerebral vascular accident.
The OSAH diagnosis is determined by the apnea and hypopnea index (AHI) over 5 events per hour of sleep, obtained through polysomnography, a “gold standard” test for the diagnostic of sleep disorders. Such index allows the classification of the OSAH into mild, moderate and severe.4,6
The literature indicates that the OSAH risk factors are: male gender, being over 50 years of age, obesity, increase of the neck volume, craniofacial alterations, genetic factors, drinking and smoking habits, consumption of drugs such as sedatives and hypnotics.7
The OSAH classic manifestation is as excessive daytime sleepiness (EDS). Clinically defined as a difficulty to maintain a desired level of alertness or as an excessive amount of sleep, the EDS is reported by patients as complaints about tiredness and lack of energy.3,5
The EDS hinders the practice of daily activities, causes memory and concentration decrease, learning disabilities, tendency to nervousness and/or depression, headache, hyperactivity (in children), social embarrassment, social issues and sexual dysfunction. It can also be manifested as a difficulty to keep one’s attention and vigil while performing monotonous tasks such as watch TV or read a book.4,8
The Epworth Sleepiness Scale (ESS) is largely used to subjectively assess the EDS. The ESS was developed by Johns in 1991 in the form of a self-assessment questionnaire, which evaluates the probability of falling asleep in the eight situations comprising daily activities such as reading, watching TV, sitting in any public place, talking to someone and or after a meal, among other situations. The global score ranges from 0 to 24, and when over 10, the presence of the EDS is suggested.4,9
Both the EDS and the OSAH are commonly associated to automobile, domestic and labor accidents, as well as the worsening and or the beginning of cardiac diseases that lead to a high level of death rates. Given that, the importance of carrying out this study is in the necessity of enhancing the knowledge of health professionals and society towards the issues concerning the EDS and OSAH, which rapidly become a public health issue and still remain relatively unknown.
Therefore, the objective of this study was to verify the prevalence of the EDS in patients with sleep breathing disorders, as well as investigate the sensibility and specificity of the ESS in detecting the presence of the OSAH. The aim was also to correlate the AHI with the EDS degree, and age with the OSAH severeness and with the degree of excessive daytime sleepiness.
Method
A cross-sectional study was carried out with a retrospective data collection performed at the Sleep Disorders Treatment Center (RespirAR), in partnership with the Sleep Medicine Center (MEDSONO).
Data was collected at RespirAR through an analysis of medical reports by using a data collection form, filled out by the researchers, which contained items concerning the patient’s profile (gender, age), polysomnography study data (AHI) and the Epworth Scale (EDS).
Patients considered for this study were adults of both genders that have been admitted at RespirAR between January 2009 and June 2013, had taken the Nocturnal Polysomnography Test and the Epworth Scale questionnaire. Patients ruled out from this study were the ones when the administration of the Epworth Scale test was longer than six months from undergoing the Polysomnography Test.
Subjects were divided into two groups according to the AHI, following the criteria established by the International Classification of Sleep Disorders6: G1, patients not diagnosed with OSAH (AHI < 5 events/h), characterizing the control group; and G2, patients with a confirmed diagnosis of mild OSAH (AHI > 5 events/h). G2 was then divided into three subgroups: G2.1, patients with mild OSAH (AHI between 5 and 15 events/h); G2.2, patients with moderate OSAH (AHI between 15 and 30 events/h); and G2.3, patients with severe OSAH (AHI > 30 events/h).
For the descriptive analysis of the data, averages, standard deviation and 2×2 tables to relate the qualitative data through Microsoft Excel 2013 have been used. The statistical analysis was obtained from the coefficient from the Pearson Correlation, which determines the linear relationship between two random variables to verify the existence of a positive or negative correlation. The software used was the Statistical Package for the Social Sciences (SPSS Statistics), version 20.0. A p=≤ 0.05 significance has been considered.
The ESS sensibility was calculated by dividing the number of true positive patients (TP), which corresponds to the patients that have the EDS and not the OSAH, and by also adding up TP and false positive patients (FP). That is, patients who have the EDS and not the OSAH is expressed by the following formula: SENS = TP/TP+FP. By contrast, the EDS specificity was calculated by dividing the number of true negatives (TN), that is, the patients that do not have the EDS and have not been also diagnosed with the OSAH, by the sum of the number of TN and false negatives (FN), which corresponds to the group of patients who have not been diagnosed with the EDS, but have OSAH, expressed by the following formula: SPE = TN/TN+FN.
The present study followed the rules and guidelines of the Resolution 466/12, being its conduction approved by the EMESCAM Ethics and Research Committee, under no. 044/2010.
Results
104 medical reports have been analyzed, and 39 ruled out from this study, in accordance with the exclusion criteria, with a remaining sample of 65 reports.
Based on the AHI, the sample was divided into G1 or control group, composed of 11 patients diagnosed with OSAH (17%) and G2, a group with a confirmed OSAH diagnostic, composed of 54 patients (83%). The latter were then divided into three subgroups: G2.1 with 3 patients (6%), with mild OSAH; G2.2 with 13 patients (24%) with moderate OSAH; and G2.3 with 38 patients (70%), with severe OSAH. Table 1 shows the characteristics of the total sample studied and of groups G1 and G2, separately.
Table 1: sample characterization
| Total Sample | G1 | G2 | ||
| AHI | 34,31 ± 25,11 | 2,07 ± 1,56 | 40,88 ± 18,78 | |
| Age* | 55,18 ± 15,76 | 46,68 ± 13,41 | 56,73 ± 15,18 | |
| ESS | 9,63 ± 4,79 | 11,09 ± 3,73 | 9,33 ± 4,96 | |
| Gender | M | 68% | 36% | 74% |
| F | 32% | 64% | 26% | |
| *Sample: n=57; G1: n= 9; G2: n= 48; ESS = Epworth Sleepiness Scale; AHI = Apnea/Hypopnea Index | ||||
| Source: The author | ||||
In the association between OSAH and EDS, a prevalence of 52% (34) of patients with EDS has been found in the total sample, when separately analyzed. Out of the 54 patients diagnosed with OSAH (G2), 27 (50%) had EDS. As for G1, the control group, the EDS was present in 7 (64%) of the patients (n=11), according to what is shown in Table 2.
Table 2: Association between OSAH and EDS
| OSAH and EDS | Yes | No | Total |
| Yes (G2) | 27 | 27 | 54 |
| No (G1) | 7 | 4 | 11 |
| Total | 34 | 31 | 65 |
OSAH = obstructive sleep apnea/hypopnea syndrome
EDS = Excessive daytime sleepiness
Upon drawing a relationship between the presence of SDE and OSAH severeness, the following result was obtained: for the G2.1 group, mild OSAH (n=3), 2(66.6%) patients have been diagnosed with SDE, for the G2.2, moderate OSAH (n=13), 6 (46.1%) patients diagnosed with SDE and for the G2.3 group, severe OSAH (n=38), 19 (50%) found with SDE, as summarized in tables 3, 4 and 5.
Table 3: Association between mild OSAH and EDS
| Mild OSAH and SDE | Yes | No | Total |
| Yes (G2.1) | 2 | 1 | 3 |
| No | 32 | 30 | 62 |
| Total | 34 | 31 | 65 |
| OSAH = Obstructive Sleep Apnea/Hypopnea syndrome; EDS = Excessive Daytime Sleepiness
Source: The author |
|||
Table 4: Association between moderate OSAH and EDS
| Moderate OSAH and EDS | Yes | No | Total | |||
| Yes (G2.2) | 6 | 7 | 13 | |||
| No | 28 | 24 | 52 | |||
| Total | 34 | 31 | 65 | |||
| OSAH = obstructive sleep apnea/hypopnea syndrome
EDS = Excessive Daytime Sleepiness |
||||||
| Source: The author | ||||||
Table 5: Association between severe OSAH and EDS
| Severe OSAH and EDS | Yes | No | Total |
| Yes (G2.3) | 19 | 19 | 38 |
| No | 15 | 12 | 27 |
| Total | 34 | 31 | 65 |
| OSAH = Obstructive Sleep Apnea/Hypopnea syndrome; EDS = Excessive Daytime Sleepiness | |||
| Source: The author | |||
The sensibility and specificity of the Epworth Sleepiness Scale (ESS) in detecting mild, moderate and severe OSAH is represented in table 6.
Table 6: ESS sensibility and specificity and OSAH severeness
| OSAH severeness | n | ESS | |
| Sensibility | Specificity | ||
| Mild OSAH | n=3 | 5.8% | 96% |
| Moderate OSAH | n=13 | 17.6% | 77.4% |
| Severe OSAH | n=38 | 55.8% | 38.7% |
| OSAH = Obstructive Sleep Apnea/Hypopnea syndrome; ESS = Epworth Sleepiness Scale | |||
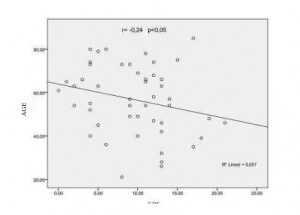
When performing the Pearson correlation between the AHI and with the EDS degree out of the total sample, statistically significant data was not found (p = > 0.05). A similar case occurred in the correlation between the AHI and the age of analyzed patients in the present study. However, when correlating age and EDS, a weak and negative correlation was found (r = – 0.24) and statistically significant (p = > 0.05), as shown in graph 1.
Graph 1: Correlation between AGE and EDS
Discussion
Tangerina et al10, in a similar study, have studied the polysomnographic findings of 45 patients diagnosed with and without OSAH, reaching an AHI general average of 30.8 ± 31.9 events per hour of sleep, a value close to the average shown in the present study, which is of 34.31 ± 25.11. Once again similar to this study, the authors divided their total sample into patients with and without OSAH, that is, patients with an AHI > 5 events/h < 5 events/h, respectively. As for the OSAH group, a total of 35 (78%) patients, the average AHI found was of 38.7 ± 32. As for the group not diagnosed with OSAH, 10 (22%) patients, 2.96 ± 1.6, while in this group the percentage found between patients diagnosed and not diagnosed with OSAH was of 83% against 17%. The AHI average for the OSAH group was of 40,88 ± 18,78 and for the group not diagnosed with OSAH, 2.07 ± 1.56, once again showing the similarities in the findings between both studies. In patient stratification, according to the OSAH severeness, the G2 group was divided into two subgroups, in which it was found a 6% (3) mild OSAH prevalence, 24% (13) of moderate and 70% (38) of the severe one. Knorst, Souza and Martinez11 when analyzing 300 patients seen at a sleep clinic with a confirmed OSAH diagnosis, have found similar results upon dividing their sample by using the same criteria applied in this study. The prevalence found was of: 12% (36) of patients with mild OSAH, 17.3% (52) for moderate and 69.3% (208) for severe.
Still analyzing the patient profile variable, it could be noted that concerning age, the average obtained in this study was of 55.18 ± 15.76, varying between 21 and 85 years old, which corroborates with the studied literature that underlines the ages between 50 and 60 years old as important risk factors for the development of OSAH7. However, more recent studies have shown a growing age average even narrower, as per the study carried out by Rodrigues et al12 in which 112 patients seen in an OSAH ambulatory were studied and the average age found was of 47.95 ± 11.25 with a range between 17 to 77 years old.
When age averages were compared between groups G1 and G2, it was found a difference of a little more than 10 years old between them (46.68 ± 13.41 vs. 56.73 ± 15.18 years old), a datum that conflicts with the studies of Carvalho7, who affirms that growing old is directly proportionate to the increase in the OSAH incidence.
The age effect on the prevalence of OSAH deserves enlightenment. However, studies tend to be cohesive when affirming that there is a positive correlation among age, obesity and circumference of the neck. In other words, the weight and circumference of the neck, that make up the list of risk factors for OSAH, proportionally increase as one gets older, which also makes it a risk factor for the disease.
As for gender, male patients make up 68% (44) of this study’s sample, being such average even higher when assessing the group diagnosed with OSAH, G2, out of which 74% of the sample were male subjects. Alternatively, when assessing the control group, G1, only 36% of the patients were male. Daltro et al14 have found a percentage fairly close to the latter. Among the 1,595 patients at the Sleep Laboratory of the Portuguese Hospital in Salvador, state of Bahia, Brazil, 71.7% were male. In another study, Dal-Fabbro et al2 have analyzed 50 patients with a polysomnographic-based confirmed OSAH test and, among those subjects, 66% were of the male gender; once again showcasing the similarities between the results obtained in this study and the ones from the literature.
However, Malhotra and White15, in a bibliographic review of the literature, have highlighted that although more recent studies have confirmed that OSAH affects more subjects of the male gender, attention must be paid to the fact that women may be being underdiagnosed. Collop, Adkins and Phillips16 and Musmam17 still add by saying that the sleep apnea is more clinically evident in male subjects, with a more frequent snoring event and witnessed apnea. In women, apnea tends to present less specific symptoms such as sleepiness and fatigue, these being easily misunderstood with daily stress, or simply neglected, which makes such patients less often referred to polysomnography.
Regarding EDS, a 52% prevalence has been found when comparing groups. Such rate was even higher in the control groups. The averages obtained through the Epworth Sleepiness Scale also diverged when both groups were compared, having the control group, once again, obtained higher rates to the ones found in the OSAH group. This fact has demonstrated the low sensibility of the scale in screening the patients bearing such disease.
Gondim et al3 have conducted a retrospective study with 125 patients with and without OSAH and have found, among similar findings to this study’s, a prevalence of 54.4% of patients with EDS in the general population. However, when comparing the populations with moderate and severe, mild and no OSAH occurrence, the findings have demonstrated a significant higher prevalence in the first group. Also corroborating with Gondim et al3, Boari et al18 have conducted a study with 66 patients that were submitted to the polysomnography test and that also responded to the ESS. It was not found a correlation between the parameters in patients with mild and moderate OSAH. However, statistically significant values have been observed in patients with the severe form of the disease; 65% of the patients obtained abnormal values of sleepiness.
Upon correlating the AHI with the Epworth Scale scoring, a statistically significant correlation was not found. Musman et al17, when analyzing 323 patients submitted to polysomnography due to a previous suspicion of sleepiness disorder, have also not found a significant correlation between the sleepiness measured by the Epworth Scale and OSAH. The author relates the results to the scale subjectivity and performance.
In what concerns the EDS, conflicting results have often been in evidence in the literature, once sleepiness becomes a daily growing and frequent symptom throughout all individuals due to an everyday escalating demand from these subjects.
In the study conducted by Bittencourt et al19, in which 2,110 individuals from 150 different Brazilian cities were interviewed by the Datafolha institute and questioned, among various subjects, about sleeping complaints. It was found that 63% of the interviewed population has presented at least one complaint regarding sleep. Given that, it is possible to draw that a low-quality sleeping habit, associated to arduous working hours during the day, may lead such individuals to present the SDE without necessarily being OSAH bearers.
Another piece of data that confronts with the latter is when sleepiness is to be compared to the age of the individuals from the sample, a weak, negative and statistically significant correlation was obtained. That is, the younger the individual, the greater the population sleepiness rate. That leads one to ponder over the fact that the young population has presented more signs of sleepiness, even when not presenting signs of a sleep disorder.
According to Chervin9, although being a globally and widely used instrument to measure sleepiness, questions hover over the arguments of what the Epworth Sleepiness Scale actually measures. Chervin claims that all authors using such scale are certainly measuring the same matter. However, in the absence of a full understanding of the physiological process that unchains sleepiness, the best way to measure it is still vague, posing a question to the sensibility of such scale, mainly in determining a predisposition to the OSAH of any other specific disease.
Conclusion
The prevalence of excessive daytime sleepiness (SDE) in this study was of 52% in the total population. The individuals were mostly males, and the mean age was of 55.18 ± 15.76 years old, with a AHI average of 34.31 ± 25.11 events per hour of sleep and for the ESS, 9.63 ± 4.79.
Upon comparing the AHI degree with the EDS, data that cannot be incisively affirmed for not being statistically significant. The same fact is true in the correlation between the AHI and the age of patients. When comparing age with EDS, a weak and negative correlation has been found, though statistically significant.
The EDS was found in half of the patients diagnosed with OSAH, presenting low values of sensibility and specificity, besides being recurrent in mostly of the patients not diagnosed with SAHOS, leading one to believe that the Epworth Scale cannot be the sole instrument to detect such disease. In this way, that makes necessary the administration of other tests that can better predict such disorders, making clear the reference to the polysomnography test.
It is also worth highlighting the necessity of new studies on excessive daytime sleepiness to better inform the individuals bearing such illness, which is commonly related to accidents and the development of cardiovascular morbidity, which have become a key public health issue.
Acknowledgements
Special thanks to the support of the Fundação de Amparo à Pesquisa do Espírito Santo (FAPES) and to the Sleep Disorders Treatment Center (RespirAR) and to the Sleep Medicine Center – MEDSONO).
References
- Da Costa VC. Ronco primário e síndrome da apneia e hipopneia obstrutiva do sono. [Monografia Especialização em Ortodontia]. Porto Alegre – Instituto de Ciências da Saúde Funorte/Soebrás; 2010. 68p.
- Dal-Fabbro C, Chaves Junior CM, Bittencourt LRA, Tufik S. Avaliação clínica e polissonográfica do aparelho BRD no tratamento da síndrome da apneia obstrutiva do sono. Dental Press J Orthod. 2010 jan-fev;15(1):107-117.
- Gondim LMA, Matumoto LM, Melo-Júnior MACM, Bittencourt S, Ribeiro UJ. Estudo comparativo da história clínica e da polissonografia na síndrome da apneia/hipopneia obstrutiva do sono. Rev Bras Otorrinolaringol. 2007 ;73(6):733-7.
- Mancini MC, Aloe F, Tavares S. Apneia do sono em obesos. Arq Bras Endocrinol Metab. 2000 fev;44(1):81-90.
- Abreu GA, Oliveira LCL, Nogueira AR, Bloch KV. Clinical presentation: recognizing the patient with obstructive sleep apnea. Rev Bras Hipertens. 2009;16(3):164-8.
- American Academy of Sleep Medicine. International classification of sleep disorders, revised: Diagnostic and coding manual. Chicago: American Academy of Sleep Medicine, 2001.
- Carvalho VMA. Síndrome da apneia/hipopneia obstrutiva do sono. [Dissertação Mestrado em Medicina]. Covilhã: Universidade da Beira do Interior. 2008. 154p.
- Tsai SC. Excessive sleepiness. Clin Chest Med. 2010 jun;31(2):341-51.
- Chervin RD. Epworth sleepiness scale? Sleep Med. 2003;4(3):175-6.
- Tangerina RP, Martinho FL, Togeiro SM, Gregório LC, Tufik S, Bittencourt LR. Achados clínicos e polissonográficos em pacientes com obesidade classe III. Rev Bras Otorrinolaringol. 2008 jul-ago;74(4):579-82.
- Knorst MM, Souza FJFB, Martinez D. Síndrome das apnéias-hipopnéias obstrutivas do sono: associação com gênero e obesidade e fatores relacionados à sonolência. J Bras Pneumol. 2008;34(7):490-6.
- Rodrigues MM, Dibbern RS, Goulart CW, Palma RA. Correlation between the Friedman classification and the Apnea-Hypopnea Index in a population with OSAHS. Braz J Otorhinolaryngol. 2010 sep-oct;76(5):557-60.
- Martins AB, Tufik S, Moura SM. Physiopathology of obstructive sleep apnea-hypopnea syndrome. J Bras Pneumol. 2007 Jan-Feb;33(1): 93-100.
- Daltro CHC, Fontes FHO, Santos-Jesus R, Gregório PB, Araújo LMB. Obstructive sleep apnea and hypopnea syndrome (OSAHS): association with obesity, gender and age. Arq Bras Endocrinol Metab. 2006 fev;50(1):74-81.
- Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002 jul;360(9328):237-45.
- Collop NA, Adkins D, Phillips BA. Gender differences in sleep and sleep-disordered breathing. Clin Chest Med 2004 jun;25(2):257-68.
- Musman S, Passos VMA, Silva IBR, Barreto SM. Avaliação de um modelo de predição para apneia do sono em pacientes submetidos a polissonografia. J Bras Pneumol. 2011;37(1):75-84.
- Boari L, Cavalcanti CM, Bannwart SRFD, Sofia OB, Dolci JEL. Avaliação da escala de Epworth em pacientes com a Síndrome da apneia e hipopneia obstrutiva do sono. Rev Bras Otorrinolaringol. 2004 nov-dez;70(6):752-6.
- Bittencourt LRA, Santos-Silva R, Taddei JA, Andersen ML, De Melo MT, Tufik S. Sleep Complaints in the Adult Brazilian Population: A National Survey Based on Screening Questions. J Clin Sleep Med. 2009;5(5):459-463.
Authors
Gracielle Pampolim¹; Juliana Moreira Pires²; Roberta Barcellos Couto3; Roberta Ribeiro Batista4
1 Master of Public Policy and Local Development from the Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória – EMESCAM, Physiotherapist, Professor at the Physical Therapy undergraduation course at the Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória – EMESCAM.
2 Physiotherapist graduated from the Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória – EMESCAM.
3 Medical Doctor graduated from the Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória – EMESCAM. Pneumologist Physician at the Sleep Medicine Center – MEDSONO.
4 Master of Biomedical Engineering from the Vale do Paraíba University, Physiotherapist – Professor and Coordinator of the Physical Therapy undergraduation course at the Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória – EMESCAM.
Article received on April 8, 2015
Article accepted on May 9, 2016